Contact our boss directly.
Don’t wait — our boss replies within 20 minutes to all inquiries.
Submit your question now and get professional feedback, accurate pricing, and technical advice — fast.
Key Takeaways
- Overflow filter cartridges are a last-line safety barrier that prevents liquid carryover into vacuum sources, pumps, and sensitive medical equipment.
- In healthcare, “a little spill” can become contamination, biofilm, and downtime—fast.
- The right choice depends on hydrophobic media, pore structure, flow rate, and compatibility with disinfectants and sterilization routes.
- Most failures aren’t dramatic—they’re boring: wrong orientation, missed changeouts, wetting, bypass leaks.
- Treat overflow filters like insurance: cheap when you buy them, expensive when you ignore them.
Overflow filter cartridges matter in healthcare because they prevent liquid carryover—blood, saline, condensate, disinfectant—into places that should stay dry: vacuum lines, pumps, suction regulators, sensors, and downstream infrastructure. That one function quietly supports infection control, device reliability, and hospital uptime. If you remove the filter (or pick the wrong one), you invite contamination, damage, and the kind of maintenance work nobody wants to do on a Friday night. In plain terms: overflow filters are a small component with an oversized job—protecting patients and equipment by keeping fluids in their lane.
Now, let me tell you why I’m stubborn about this topic.
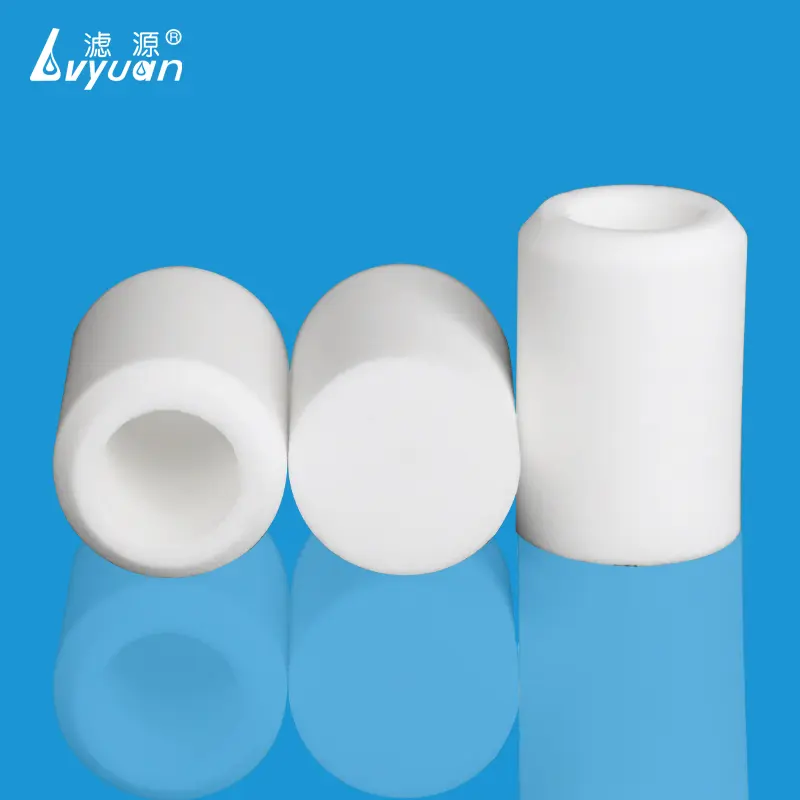
An overflow filter cartridge is a protective filter element—often hydrophobic—installed in a fluid path to stop liquid from passing beyond a certain point while still allowing airflow (or controlled venting). Think of it as a “doorman” for a system that’s supposed to breathe, but absolutely should not drink.
A regular filter usually exists to remove particles from a fluid stream. Overflow filters are more about preventing fluid intrusion and protecting downstream equipment—especially vacuum systems and suction setups.
If you’ve ever seen a vacuum line that smells like something from a crime scene, you already understand why this matters.
Healthcare is not a forgiving environment. It’s not a factory where you can shrug off a mess and run a solvent flush. In hospitals, clinics, labs, and dialysis centers, contamination has a nasty habit of becoming a chain reaction.
Overflow events can create aerosols, wet internal surfaces, and encourage microbial growth. Once moisture and organic matter get into places designed to stay dry—like vacuum components and tubing runs—cleaning becomes complicated, verification becomes harder, and trust goes out the window.
I’m going to be blunt: filters don’t prevent every infection, and anyone promising that is selling you fantasy. But they do reduce avoidable contamination routes. And that’s the real game.
The ugliest truth in hospital maintenance is this: downtime doesn’t show up as a neat line item until it’s already painful.
Overflow filters help prevent:
When you’re buying filters, you’re not paying for plastic and pores. You’re paying for predictability.

Overflow filtration is common anywhere fluids and air share space and “oops moments” happen.
Suction canisters, wall suction regulators, portable suction units—these systems are designed to move air, but they inevitably meet fluid. An overflow filter is the guardrail that keeps that fluid from migrating into the vacuum source.
Lab instruments often have waste lines, venting paths, pressure sensing, and small pneumatic channels. A little backflow or condensation where it shouldn’t be can cause errors, contamination, or service interruptions.
Dialysis setups and related clinical equipment involve tight control of fluids and pressure. Overflow prevention becomes part of keeping systems stable and limiting contamination risks.
Reprocessing departments deal with humidity, condensate, and aggressive cleaning chemicals. Anywhere there’s a vacuum assist, venting, or suction, overflow protection is worth serious attention.

Here’s where selection goes right or wrong.
If the filter media wets out too easily, the “liquid barrier” becomes a “liquid invitation.” Hydrophobic membranes and sintered structures can be used depending on design, but the key property is the same: resist wetting while maintaining airflow.
Smaller pores generally increase barrier performance but can reduce flow and clog faster. Larger pores may flow well but may not provide the barrier you think you’re buying. The correct target depends on:
A filter that blocks overflow but chokes airflow can cause system alarms, sluggish suction, or inaccurate sensing.
Ask yourself:
Healthcare environments love disinfectants. Disinfectants love attacking the wrong polymers.
If your filter sees wipe-down chemicals, vapor exposure, or accidental splashes, compatibility becomes real. Not theoretical. Real.
Some components are single-use. Some are part of a reusable assembly. Either way, the filter has to survive the intended sterilization method (where applicable) without degrading performance.
A practical question I always ask: What changes after sterilization—flow, integrity, shedding, or wetting behavior? If nobody has data, you’re gambling.
Most failures aren’t spectacular. They’re boring, and that’s why they repeat.
Some overflow filters are directional. Install it backwards and you’ve built a very expensive placebo.
A filter that’s loaded, wetted, or fouled can restrict airflow and trigger alarms—or worse, allow bypass around seals if pressure differentials spike.
I’ve seen people obsess over pore size and ignore the fact that the connection leaks. If your sealing surface is poor, fluid will take the path of least resistance. It always does.
Humidity, condensate, surfactants, or aerosolized chemicals can change wetting behavior. That “hydrophobic” filter might be hydrophobic… until it isn’t.
If you can’t answer these, you’re not selecting a filter—you’re selecting a guess.

Here’s my favorite one-liner for leadership:
“Overflow filters are cheap insurance against contamination and downtime.”
Not glamorous. Very true.
It prevents liquid carryover into vacuum lines, pumps, or sensitive equipment while allowing airflow or venting, supporting infection control and device reliability.
They’re commonly used in suction systems, vacuum infrastructure, portable suction devices, certain lab analyzers, and other fluid-handling equipment where liquid intrusion is a risk.
Not always. Some designs provide microbial barrier performance, but many overflow filters focus primarily on stopping liquid carryover. You should verify barrier requirements and test standards for your application.
Replacement depends on usage, humidity, aerosol exposure, and overflow events. A smart rule: replace after any significant overflow incident and follow a scheduled maintenance interval based on performance monitoring (like ΔP or alarms).
Hydrophobicity, pore structure, airflow capacity, pressure drop, seal integrity, and compatibility with disinfectants and sterilization routes are usually the critical factors.
Overflow filter cartridges are not a “nice to have.” They’re the quiet bouncer standing between your healthcare equipment and a messy, expensive mess. When they’re specified correctly and maintained properly, nobody notices them—which is the highest compliment a safety component can get.
When they’re missing, undersized, incompatible, or installed wrong? Everyone notices. Usually at the worst possible time.
If you paste your Internal Links JSON, I’ll revise this draft and naturally insert 5–8+ internal links exactly per your rule: same keyword text, Markdown format, no forced placements, no invented URLs.